What Is Mci
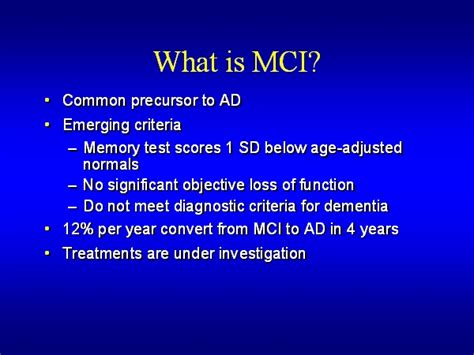
Mild cognitive impairment (MCI) is a medical condition that falls between the normal cognitive decline associated with aging and the more severe symptoms of dementia. It is characterized by subtle changes in cognitive abilities, primarily affecting memory, language, and other mental functions, but these changes are not severe enough to interfere significantly with daily life and activities.
MCI is an important topic of study and discussion in the fields of neurology and geriatrics, as it often serves as a precursor to more serious neurological disorders, particularly Alzheimer's disease. However, not all individuals with MCI will develop dementia, and some may even revert to normal cognitive functioning. Understanding MCI is crucial for early detection, intervention, and potentially slowing down the progression to dementia.
Understanding Mild Cognitive Impairment
Mild cognitive impairment is a broad term used to describe a set of symptoms that reflect a decline in cognitive abilities. These symptoms can vary widely among individuals, and not all cognitive domains are necessarily affected. Common areas of impairment include memory, language, attention, and executive function.
While memory loss is often the most noticeable symptom, other cognitive changes may also be present. For instance, some individuals with MCI may struggle with finding the right words, organizing thoughts, or planning and executing tasks. Emotional and behavioral changes can also accompany MCI, although these are less frequently discussed.
The diagnosis of MCI is made through a comprehensive assessment of cognitive function, often involving a series of tests and evaluations. These assessments are designed to differentiate MCI from normal cognitive aging and more severe forms of dementia. The evaluation process typically includes a thorough medical history, cognitive testing, and sometimes brain imaging to rule out other potential causes of cognitive decline.
Common Symptoms of MCI
- Memory Loss: Forgetting recent events, misplacing items, and struggling to recall familiar words or names.
- Language Difficulties: Challenges in finding the right words, understanding complex sentences, or expressing thoughts clearly.
- Attention and Concentration Issues: Difficulty maintaining focus, especially in noisy or distracting environments.
- Executive Function Impairment: Problems with planning, organizing, and making decisions, which can affect daily tasks and activities.
- Emotional and Behavioral Changes: Increased irritability, anxiety, or apathy; changes in social behavior or interactions.
It's important to note that these symptoms are not severe enough to disrupt daily life or cause significant functional impairment. Individuals with MCI can often still live independently and carry out their normal routines, although they may need extra time or support for certain tasks.
Causes and Risk Factors of MCI
The exact causes of MCI are not fully understood, and it is believed to result from a combination of genetic, environmental, and lifestyle factors. Some of the key risk factors associated with MCI include:
- Age: The risk of MCI increases with age, with most cases occurring in individuals over 65 years old.
- Family History: Having a first-degree relative with Alzheimer's disease or another form of dementia can increase the risk of developing MCI.
- Genetics: Certain genetic variations have been linked to an increased susceptibility to MCI and dementia.
- Lifestyle Factors: Poor diet, lack of physical activity, smoking, and excessive alcohol consumption can contribute to cognitive decline.
- Cardiovascular Health: Conditions that affect the heart and blood vessels, such as high blood pressure and high cholesterol, can increase the risk of MCI.
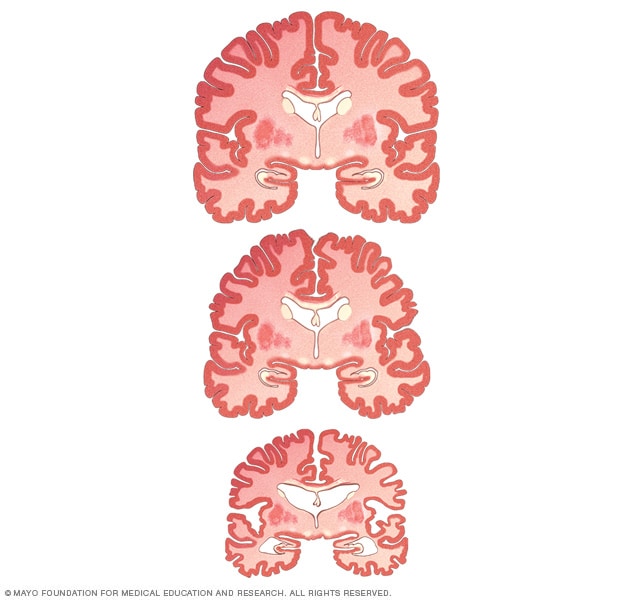
- Brain Changes: Neurodegenerative processes, such as the buildup of proteins in the brain, can lead to MCI and eventually dementia.
While some of these risk factors cannot be modified, adopting a healthy lifestyle and managing cardiovascular risk factors can potentially reduce the likelihood of developing MCI and slow down cognitive decline.
Diagnosis and Assessment of MCI
Diagnosing MCI involves a detailed evaluation of cognitive function and a thorough medical history. Healthcare professionals use various tools and tests to assess different cognitive domains, including memory, language, attention, and executive function. These assessments are typically standardized and validated to ensure accurate and consistent results.
In addition to cognitive testing, brain imaging techniques such as MRI and CT scans may be used to rule out other potential causes of cognitive decline, such as tumors, strokes, or vascular diseases. These imaging tests can also provide valuable information about brain structure and potential changes associated with MCI.
Once a diagnosis of MCI is made, healthcare providers will often recommend regular follow-up assessments to monitor the progression of symptoms and make appropriate treatment and management plans. Early detection and intervention are key to optimizing the quality of life for individuals with MCI and potentially slowing down the progression to dementia.
| Diagnostic Tool | Description |
|---|---|
| Mini-Mental State Examination (MMSE) | A widely used cognitive screening tool that assesses various domains, including orientation, memory, attention, and language. |
| Montreal Cognitive Assessment (MoCA) | A more detailed assessment that evaluates multiple cognitive domains, often used for early detection of MCI and dementia. |
| Neuropsychological Testing | Comprehensive testing to assess specific cognitive functions, often used to differentiate MCI from other neurological conditions. |
| Brain Imaging | MRI and CT scans to visualize brain structure and rule out other causes of cognitive decline. |

Managing and Treating MCI
While there is currently no cure for MCI, various strategies can be employed to manage symptoms and potentially slow down cognitive decline. The primary goals of MCI management include:
- Slowing Cognitive Decline: Implementing lifestyle interventions and medications to potentially slow the progression of cognitive impairment.
- Enhancing Cognitive Function: Engaging in activities that stimulate the brain and improve cognitive reserve, such as cognitive training and social engagement.
- Managing Symptoms: Addressing specific symptoms, such as memory loss or language difficulties, to improve daily functioning.
- Reducing Risk Factors: Managing underlying conditions and adopting a healthy lifestyle to minimize the impact of risk factors.
Lifestyle interventions play a crucial role in MCI management. These interventions include regular physical exercise, a healthy diet rich in fruits, vegetables, and omega-3 fatty acids, cognitive training and stimulation, and social engagement. Studies have shown that these lifestyle changes can improve cognitive function and potentially slow down the progression of MCI.
Lifestyle Interventions for MCI
Physical exercise has been shown to have numerous benefits for individuals with MCI. Regular aerobic exercise, such as walking, swimming, or cycling, can improve cardiovascular health, which in turn can enhance cognitive function. Additionally, strength training and balance exercises can help maintain mobility and reduce the risk of falls, which is particularly important for older adults.
A healthy diet, such as the Mediterranean-style diet, has also been linked to better cognitive outcomes. This diet is rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, while limiting processed foods and added sugars. Omega-3 fatty acids, found in fish and nuts, have been particularly associated with improved cognitive function and a reduced risk of dementia.
Cognitive training and stimulation involve engaging in activities that challenge the brain, such as puzzles, crosswords, or learning a new skill. Social engagement, through activities like volunteering, joining community groups, or participating in social events, can also provide cognitive benefits and improve overall well-being.
While lifestyle interventions are the cornerstone of MCI management, medications may also be prescribed to address specific symptoms or underlying conditions. For instance, cholinesterase inhibitors, commonly used in the treatment of Alzheimer's disease, may be beneficial for some individuals with MCI. However, the use of medications in MCI is a complex topic, and decisions should be made in consultation with healthcare professionals.
Future Implications and Research
The field of MCI research is rapidly evolving, with ongoing studies investigating various aspects of the condition. Some key areas of focus include:
- Biomarkers: Researchers are exploring the development of biomarkers to aid in the early detection and diagnosis of MCI and to predict the progression to dementia.
- Neuroimaging: Advanced brain imaging techniques are being used to understand the structural and functional changes associated with MCI and to identify potential targets for intervention.
- Lifestyle Interventions: Ongoing research is evaluating the effectiveness of various lifestyle interventions, such as diet, exercise, and cognitive training, in slowing down cognitive decline and improving overall brain health.
- Pharmacological Treatments: Clinical trials are underway to test the efficacy of new medications and therapies for MCI, with the goal of finding treatments that can modify the course of the disease.
- Prevention Strategies: Public health initiatives are being developed to promote brain health and reduce the risk of MCI and dementia through education, community programs, and policy changes.
As our understanding of MCI deepens, healthcare professionals and researchers are hopeful that early detection, combined with effective interventions, can significantly improve the lives of individuals with MCI and potentially delay or prevent the onset of dementia.
Key Takeaways
- Mild cognitive impairment (MCI) is a condition characterized by subtle cognitive changes that are not severe enough to interfere with daily life.
- MCI is often a precursor to more serious neurological disorders, particularly Alzheimer’s disease, but not all individuals with MCI will develop dementia.
- Early detection through comprehensive cognitive assessments and brain imaging is crucial for timely intervention and potentially slowing down the progression to dementia.
- Lifestyle interventions, including regular physical exercise, a healthy diet, cognitive training, and social engagement, are key strategies for managing MCI and potentially slowing cognitive decline.
- Ongoing research in the field of MCI is focused on early detection, effective interventions, and the development of new treatments to modify the course of the disease.
What is the difference between MCI and normal cognitive aging?
+Normal cognitive aging involves subtle changes in cognitive abilities that are expected as we get older. These changes may include mild memory lapses, slower processing speed, and occasional word-finding difficulties. However, these changes do not significantly interfere with daily life or activities. In contrast, MCI is characterized by more noticeable cognitive changes that go beyond normal aging. These changes can affect memory, language, attention, and other mental functions, and they may require extra time or support for daily tasks.
Can MCI be prevented or reversed?
+Currently, there is no definitive way to prevent or reverse MCI. However, adopting a healthy lifestyle, including regular physical exercise, a nutritious diet, cognitive stimulation, and social engagement, can potentially reduce the risk of developing MCI and slow down cognitive decline. While these lifestyle interventions may not reverse existing cognitive impairment, they can improve overall brain health and potentially delay the progression to dementia.
How is MCI diagnosed?
+Diagnosing MCI involves a comprehensive evaluation of cognitive function. Healthcare professionals use a variety of tools and tests to assess different cognitive domains, such as memory, language, attention, and executive function. These assessments are typically standardized and validated to ensure accurate results. In addition, brain imaging techniques like MRI and CT scans may be used to rule out other potential causes of cognitive decline. The diagnosis of MCI is made based on the presence of specific cognitive symptoms that are not severe enough to meet the criteria for dementia.
What are the potential outcomes of MCI?
+The potential outcomes of MCI can vary widely among individuals. Some individuals with MCI may revert to normal cognitive functioning over time, while others may experience a progression to dementia, particularly Alzheimer’s disease. However, it’s important to note that not all cases of MCI will lead to dementia. Early detection, timely intervention, and effective management of MCI can potentially slow down the progression to dementia and improve overall quality of life.



