Staphylococcus
Staphylococcus, often referred to as "staph," is a group of bacteria that can cause a wide range of infections and diseases in humans and animals. These bacteria are ubiquitous in our environment and can be found on the skin, in the nose, and in various mucous membranes. While most strains of Staphylococcus are relatively harmless, certain types can lead to serious and potentially life-threatening conditions. Understanding the different species, their characteristics, and the diseases they cause is crucial for effective healthcare and infection control.
The Genus Staphylococcus: An Overview

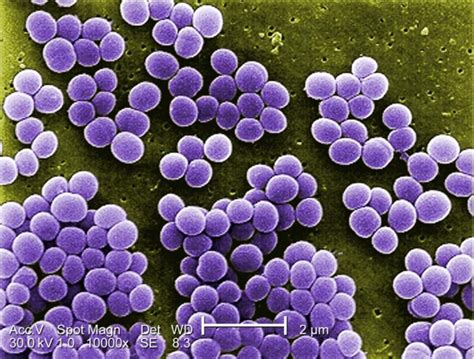
The genus Staphylococcus belongs to the Staphylococcaceae family within the phylum Firmicutes. These bacteria are gram-positive cocci, appearing as clusters resembling grapes under a microscope. Their ability to produce a thick layer of peptidoglycan in their cell walls contributes to their resilience and resistance to certain antibiotics.
Staphylococci are facultative anaerobes, meaning they can survive in both aerobic and anaerobic environments. This adaptability allows them to colonize various body sites and thrive in diverse environmental conditions.
Key Characteristics of Staphylococci
- Coagulase Production: Staphylococci can be classified based on their ability to produce coagulase, an enzyme that clots plasma. Coagulase-positive strains, such as Staphylococcus aureus, are more virulent and cause more severe infections.
- Hemolysis: Some species, like Staphylococcus aureus, can produce hemolysins, which are substances that cause the breakdown of red blood cells.
- Biofilm Formation: Staphylococci have the ability to form biofilms, which are complex structures that protect them from antibiotics and the host’s immune system. This makes treating staphylococcal infections more challenging.
Common Staphylococcal Species and Their Impact

While there are numerous species within the genus Staphylococcus, a few stand out for their clinical significance and impact on human health.
Staphylococcus aureus: A Leading Cause of Infections
Staphylococcus aureus, often referred to as “S. aureus,” is a prominent pathogen responsible for a wide spectrum of infections. It is a coagulase-positive strain, which means it can produce coagulase, enhancing its virulence.
| Disease | Description |
|---|---|
| Skin and Soft Tissue Infections | S. aureus is a common cause of skin infections like boils, impetigo, and cellulitis. These infections can range from mild to severe, and sometimes require hospitalization. |
| Food Poisoning | Ingesting food contaminated with S. aureus can lead to rapid-onset symptoms such as nausea, vomiting, and diarrhea. This is due to the production of enterotoxins by the bacteria. |
| Pneumonia | Infections of the lower respiratory tract, such as pneumonia, can occur when S. aureus spreads from the nose and throat to the lungs. |
| Endocarditis | When S. aureus infects the inner lining of the heart chambers and valves, it can cause endocarditis, a serious and potentially fatal condition. |

Staphylococcus epidermidis: A Common Colonizer
Staphylococcus epidermidis is a coagulase-negative strain that is a normal resident of the skin and mucous membranes. While it is typically harmless in healthy individuals, it can cause infections in certain situations.
| Infection Type | Description |
|---|---|
| Device-Related Infections | S. epidermidis is a frequent cause of infections associated with medical devices such as catheters and prosthetic joints. Its ability to form biofilms on these devices makes it challenging to treat. |
| Endocarditis | Like S. aureus, S. epidermidis can also cause endocarditis, particularly in individuals with heart valve defects or those who have undergone valve replacement surgery. |
Other Notable Staphylococcal Species
- Staphylococcus saprophyticus: A common cause of urinary tract infections, especially in young, sexually active women.
- Staphylococcus haemolyticus: This species is often associated with bloodstream infections and surgical site infections.
- Staphylococcus lugdunensis: Known for causing aggressive skin and soft tissue infections, as well as endocarditis.
Diagnosis and Treatment of Staphylococcal Infections
Diagnosing staphylococcal infections typically involves a combination of clinical evaluation, laboratory tests, and, in some cases, imaging studies. The choice of treatment depends on the specific species involved and the severity of the infection.
Diagnostic Approaches
- Culture and Sensitivity Testing: Growing the bacteria in a laboratory to identify the specific species and determine its antibiotic susceptibility.
- Molecular Techniques: These methods, including PCR, can rapidly identify staphylococcal species and detect resistance genes.
- Imaging: For deep-seated infections, imaging techniques like CT scans and MRI may be used to visualize the extent of the infection.
Treatment Strategies
The treatment of staphylococcal infections often involves the use of antibiotics. However, the rise of antibiotic-resistant strains, particularly methicillin-resistant Staphylococcus aureus (MRSA), has made treatment more complex.
- Antibiotic Selection: The choice of antibiotic depends on the specific species and its susceptibility profile. For MRSA, vancomycin or other last-resort antibiotics may be necessary.
- Infectious Disease Specialists: For complex or severe cases, consultation with an infectious disease specialist is recommended to ensure appropriate treatment.
- Surgical Intervention: In cases of deep-seated infections or abscesses, surgical drainage may be required.
Prevention and Control of Staphylococcal Infections
Preventing staphylococcal infections is a multifaceted approach that involves both personal and institutional measures.
Personal Hygiene and Prevention
- Hand Hygiene: Regular handwashing with soap and water or the use of alcohol-based hand sanitizers is crucial to prevent the spread of staphylococci.
- Wound Care: Proper care of cuts, scrapes, and wounds can prevent staphylococcal infections from developing.
- Food Safety: Practicing good food hygiene can prevent staphylococcal food poisoning.
Infection Control in Healthcare Settings
- Isolation and Contact Precautions: Implementing strict isolation measures for patients with known or suspected staphylococcal infections can prevent the spread to other patients.
- Healthcare Worker Hygiene: Encouraging healthcare workers to practice good hand hygiene and wearing personal protective equipment (PPE) can reduce the risk of transmission.
- Environmental Cleaning: Regular cleaning and disinfection of medical equipment and surfaces are essential to prevent the spread of staphylococci.
Future Perspectives and Challenges

The ongoing challenge of antibiotic resistance in staphylococci, particularly MRSA, remains a significant concern. The development of new antibiotics and alternative treatment strategies, such as phage therapy and antimicrobial peptides, is an active area of research.
Additionally, the role of staphylococci in biofilms and their ability to form complex communities with other bacteria present unique challenges for treatment and eradication. Understanding these microbial interactions and developing targeted approaches will be crucial in the fight against staphylococcal infections.
How can I differentiate between a harmless staphylococcal skin infection and a more serious one?
+While many staphylococcal skin infections are mild and can be managed with over-the-counter treatments, more severe infections may present with increased redness, swelling, warmth, and pain. If you notice any of these signs or if the infection is not improving, it’s important to seek medical advice.
What are the signs and symptoms of staphylococcal food poisoning?
+Staphylococcal food poisoning typically presents with sudden onset of nausea, vomiting, and diarrhea within a few hours of consuming contaminated food. Abdominal cramps and fever may also occur. These symptoms usually resolve within 24 to 48 hours.
How can I protect myself from staphylococcal infections in a healthcare setting?
+In healthcare settings, it’s important to follow good hand hygiene practices, avoid sharing personal items, and ensure that medical equipment is properly sanitized. If you are visiting someone with a known staphylococcal infection, follow any isolation precautions and wear personal protective equipment as recommended by healthcare professionals.



