Marfan Connective Tissue Disorder

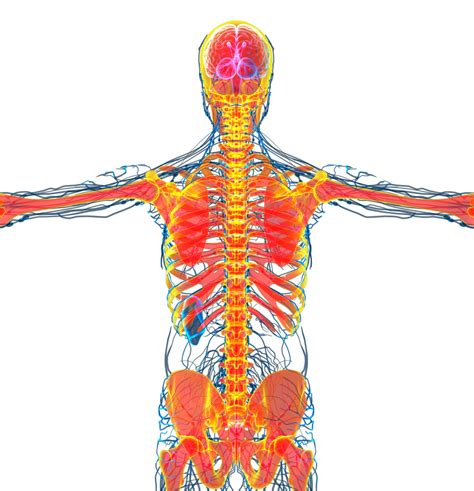
Marfan syndrome is a rare and complex genetic disorder that affects the body's connective tissue. Connective tissue provides strength and flexibility to various structures in the body, including bones, ligaments, tendons, cartilage, and blood vessels. This article aims to delve into the intricacies of Marfan syndrome, exploring its causes, symptoms, diagnosis, and management strategies.
Understanding Marfan Syndrome
Marfan syndrome is caused by a mutation in the FBN1 gene, which provides instructions for making a protein called fibrillin-1. Fibrillin-1 is a crucial component of connective tissue, playing a vital role in maintaining its integrity and elasticity. When this gene is mutated, it leads to an abnormal production of fibrillin-1, resulting in weakened connective tissue throughout the body.
This disorder follows an autosomal dominant pattern of inheritance, meaning that an affected individual has a 50% chance of passing the faulty gene to each of their children. However, it's important to note that approximately 25-30% of cases arise from spontaneous mutations, where neither parent carries the altered gene.
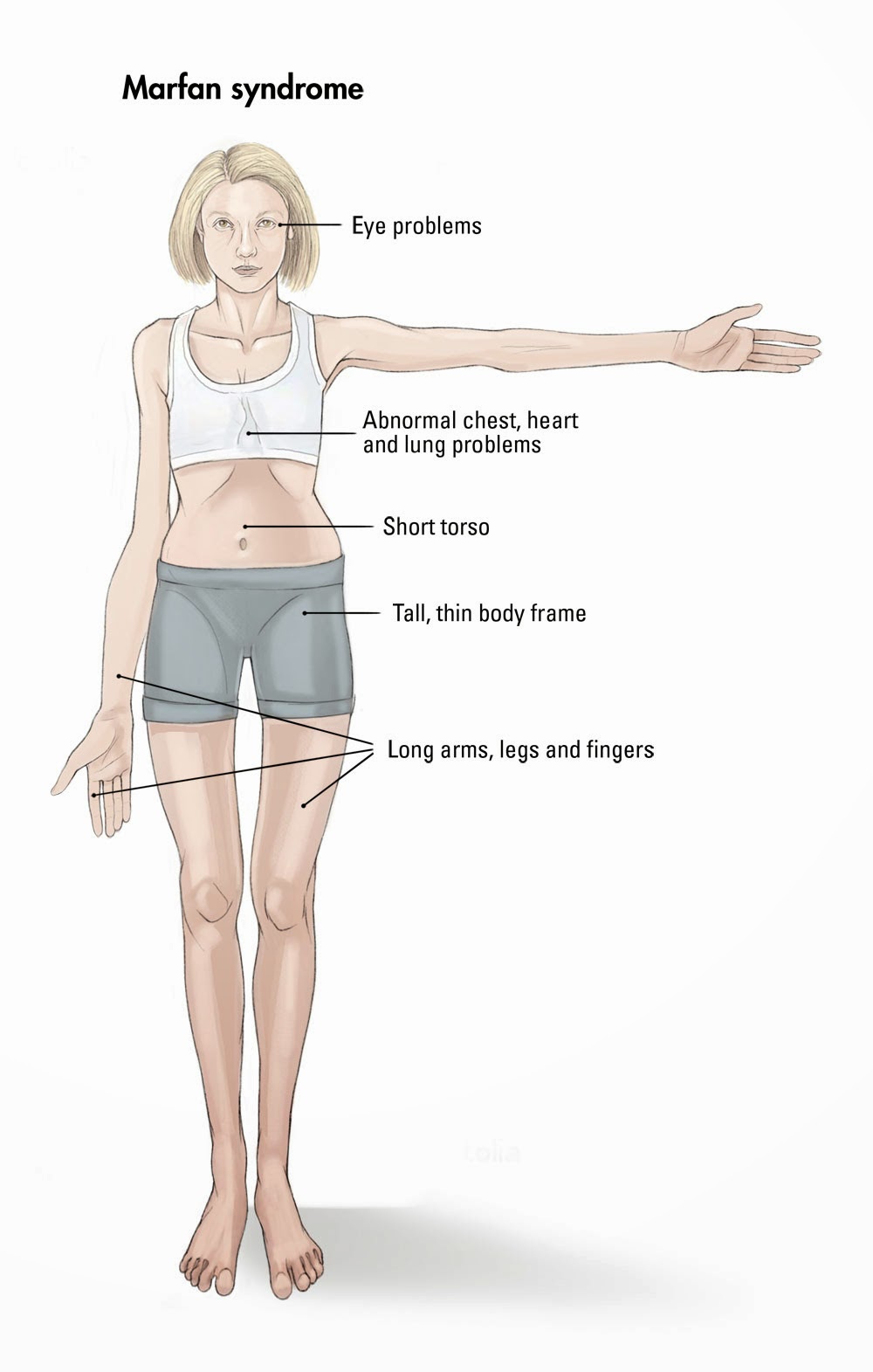
The impact of Marfan syndrome varies widely among individuals, even within the same family. Some people experience mild symptoms, while others face more severe health challenges. Common features of Marfan syndrome include:
- Tall and slender build with long limbs and fingers.
- Abnormally shaped chest with a protruding or sunken sternum.
- Eye problems, such as nearsightedness, dislocation of the lens, and early cataract formation.
- Heart problems, including mitral valve prolapse, aortic regurgitation, and aortic aneurysm.
- Skeletal issues like scoliosis, curvature of the spine, and joint hypermobility.
- Lung conditions, including spontaneous pneumothorax (collapsed lung) and sleep apnea.
Diagnosis and Screening
Diagnosing Marfan syndrome can be complex and often involves a multidisciplinary approach. Healthcare providers typically consider a combination of clinical findings, family history, and genetic testing to make a diagnosis. The Ghent Nosology, a set of diagnostic criteria, is commonly used to identify Marfan syndrome.
Key diagnostic criteria include:
- Skeletal involvement (such as tall stature, arm span to height ratio, wrist and thumb signs, etc.)
- Ocular findings (dislocated lens, myopia, etc.)
- Cardiac abnormalities (aortic root dilation, mitral valve prolapse, etc.)
- Family history of Marfan syndrome
Genetic testing for the FBN1 gene mutation can provide a definitive diagnosis, although negative results do not rule out Marfan syndrome entirely, as not all genetic changes are currently detectable.
Management and Treatment
There is no cure for Marfan syndrome, but with early diagnosis and appropriate management, individuals with this condition can lead fulfilling lives. The primary goal of treatment is to prevent or slow down the progression of life-threatening complications, particularly those affecting the heart and blood vessels.
Cardiac Management
Regular cardiac evaluations are crucial for individuals with Marfan syndrome. These may include echocardiograms, MRI scans, and electrocardiograms to monitor the heart’s structure and function. Beta-blockers are often prescribed to reduce the workload on the heart and lower blood pressure, which can help prevent aortic dilation and dissection.
In cases where the aortic root dilates significantly or dissection occurs, surgical intervention may be necessary. This can involve procedures like aortic root replacement or aortic valve repair/replacement.
Ophthalmologic Care
Eye care is an essential aspect of managing Marfan syndrome. Regular eye exams can help detect and manage issues such as dislocated lenses, myopia, and early cataract formation. Corrective lenses or contact lenses may be prescribed to improve vision, and in some cases, surgical interventions like lens replacement may be required.
Orthopedic Management
Orthopedic specialists play a vital role in managing skeletal issues associated with Marfan syndrome. Scoliosis and chest deformities may require bracing or, in severe cases, surgical correction. Joint hypermobility can be managed through physical therapy and exercises to strengthen the supporting muscles.
Additionally, individuals with Marfan syndrome should take precautions to avoid injury, as their connective tissue is more susceptible to damage. Contact sports and activities with a high risk of injury should be avoided.
Pulmonary Care
Pulmonary complications, such as pneumothorax and sleep apnea, can be managed through close monitoring and treatment. In the case of pneumothorax, surgical procedures like pleurodesis or pleurectomy may be considered to prevent recurrence.
Psychosocial Support
Living with a chronic condition like Marfan syndrome can impact an individual’s emotional well-being. Access to psychological support and counseling can help individuals cope with the challenges of the condition and improve their overall quality of life.
Prognosis and Long-Term Outlook
The prognosis for individuals with Marfan syndrome has improved significantly over the years due to advancements in medical care. With proper management and regular monitoring, many people with Marfan syndrome can expect a normal life expectancy. However, it’s crucial to maintain a proactive approach to healthcare to minimize the risk of complications.
Regular follow-ups with a team of healthcare professionals, including cardiologists, ophthalmologists, orthopedists, and genetic counselors, are essential for long-term management. Additionally, patient support groups and online communities can provide valuable resources and a sense of community for individuals living with Marfan syndrome.
Research and Future Directions
Ongoing research continues to deepen our understanding of Marfan syndrome and its management. Genetic research aims to identify additional genes involved in the disorder and develop targeted therapies. Clinical trials are exploring the use of medications to slow down the progression of aortic root dilation and other cardiac complications.
Additionally, efforts are being made to improve diagnostic accuracy and develop guidelines for the optimal management of Marfan syndrome. These initiatives aim to ensure that individuals with this condition receive the best possible care, improving their quality of life and overall health outcomes.
| Statistical Fact | Description |
|---|---|
| Prevalence | Marfan syndrome affects approximately 1 in 5,000 individuals worldwide. |
| Gender Ratio | The condition affects males and females equally. |
| Age of Onset | Symptoms typically become apparent during childhood or adolescence, but some may not be noticeable until adulthood. |
Can Marfan syndrome be prevented or cured?
+Currently, there is no known way to prevent or cure Marfan syndrome. However, with early diagnosis and proper management, individuals can lead healthy lives and prevent life-threatening complications.
How is Marfan syndrome inherited?
+Marfan syndrome follows an autosomal dominant pattern of inheritance. This means that if one parent has the condition, there is a 50% chance that each child will inherit the altered gene. However, it’s important to note that about 25-30% of cases arise from spontaneous mutations.
Are there any lifestyle modifications that can help manage Marfan syndrome?
+Yes, adopting a healthy lifestyle can significantly benefit individuals with Marfan syndrome. This includes regular exercise (with precautions to avoid injury), a balanced diet, maintaining a healthy weight, and avoiding activities with a high risk of injury. Smoking should also be avoided as it can worsen vascular complications.



