Hepatic Cirrhosis Of The Liver
Hepatic cirrhosis, a complex and progressive liver disease, poses significant health challenges worldwide. This condition, characterized by the gradual replacement of healthy liver tissue with scar tissue, demands attention due to its potential life-threatening complications. In this comprehensive article, we delve into the depths of hepatic cirrhosis, exploring its causes, symptoms, diagnosis, treatment options, and the critical role of early intervention. By unraveling the intricacies of this disease, we aim to empower readers with knowledge and understanding, fostering better health outcomes and a brighter future for those affected.
Unraveling Hepatic Cirrhosis: A Comprehensive Overview
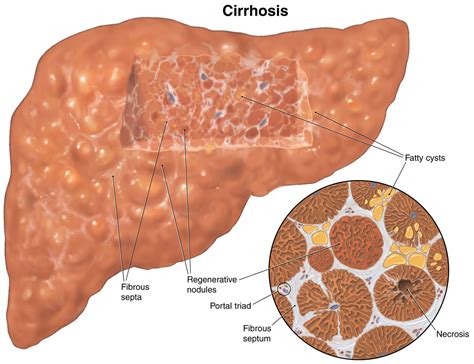
Hepatic cirrhosis, a chronic liver condition, arises from a myriad of factors, with chronic alcohol abuse and viral hepatitis taking center stage as the primary causes. This debilitating disease progresses over time, often leading to irreversible damage if left untreated. The liver, a vital organ responsible for detoxification, protein synthesis, and nutrient processing, undergoes significant structural changes during cirrhosis. Healthy liver tissue gives way to scar tissue, impeding the organ’s functionality and resulting in a range of debilitating symptoms.
The symptoms of hepatic cirrhosis are diverse and can vary in severity. Common manifestations include fatigue, loss of appetite, weight loss, and abdominal pain. As the disease advances, more severe symptoms may arise, such as jaundice (yellowing of the skin and eyes), fluid retention in the abdomen (ascites), and mental confusion or even coma (hepatic encephalopathy). These symptoms underscore the urgency of seeking medical attention, as early diagnosis and intervention are crucial for managing the condition and preventing further deterioration.
Causes and Risk Factors
The onset of hepatic cirrhosis is typically associated with long-term liver damage. Chronic alcohol abuse stands as one of the leading culprits, as excessive alcohol consumption can induce inflammation and scarring in the liver over time. Viral hepatitis, particularly hepatitis B and C, also poses a significant risk, as these viruses can infect and damage liver cells, leading to cirrhosis in some individuals.
Other factors contributing to the development of hepatic cirrhosis include non-alcoholic fatty liver disease (NAFLD), a condition characterized by fat accumulation in the liver, often linked to obesity and metabolic disorders. Autoimmune hepatitis, where the body's immune system attacks its own liver cells, and certain genetic disorders like hemochromatosis (excess iron accumulation in the body) are also potential triggers. Additionally, chronic conditions such as primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) can lead to cirrhosis by causing progressive damage to the bile ducts.
Understanding these risk factors is crucial for identifying individuals who may be susceptible to hepatic cirrhosis. Early recognition and lifestyle modifications, such as alcohol cessation and weight management, can play a pivotal role in preventing the onset or progression of this debilitating disease.
Diagnosis and Clinical Assessment
Diagnosing hepatic cirrhosis involves a meticulous clinical evaluation and a battery of diagnostic tests. Healthcare providers typically initiate the diagnostic process by conducting a comprehensive medical history review and physical examination. This initial assessment aims to identify symptoms, assess liver function, and rule out other potential causes of liver damage.
Blood tests play a pivotal role in diagnosing hepatic cirrhosis. These tests can reveal elevated liver enzymes, indicating liver damage, and assess the presence of viral hepatitis or other underlying conditions. Imaging studies, such as ultrasound, CT scans, or MRI, provide visual insights into the liver's structure, helping to detect abnormalities and assess the extent of scarring.
In some cases, a liver biopsy may be recommended to confirm the diagnosis and determine the severity of cirrhosis. This procedure involves obtaining a small tissue sample from the liver, which is then examined under a microscope to assess the extent of scarring and identify any underlying liver conditions. The results of these diagnostic tests, coupled with clinical symptoms and medical history, enable healthcare professionals to establish a definitive diagnosis and tailor an appropriate treatment plan.
Navigating Treatment Options: Managing Hepatic Cirrhosis
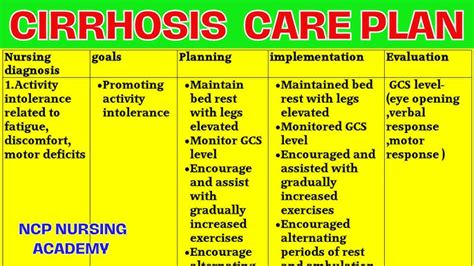
The management of hepatic cirrhosis is a multifaceted approach, focusing on addressing the underlying cause, alleviating symptoms, and preventing further liver damage. Treatment strategies are tailored to the individual’s specific needs and the stage of the disease. Here, we delve into the key aspects of managing hepatic cirrhosis, from lifestyle modifications to medical interventions and the importance of ongoing care.
Lifestyle Modifications and Self-Care
Lifestyle modifications are pivotal in managing hepatic cirrhosis and preventing further liver damage. For individuals with alcohol-related cirrhosis, complete abstinence from alcohol is imperative. This lifestyle change can halt the progression of the disease and even lead to partial liver healing in some cases. Additionally, adopting a healthy diet and maintaining a balanced weight are essential for managing non-alcoholic fatty liver disease (NAFLD), a common contributor to cirrhosis.
A liver-friendly diet, rich in antioxidants and nutrients, can support liver function and overall health. This includes incorporating fruits, vegetables, whole grains, and lean proteins into daily meals. It's also crucial to limit the intake of processed foods, sugary beverages, and saturated fats, as these can exacerbate liver inflammation and impair its function. Regular exercise, when cleared by a healthcare provider, can also play a vital role in managing weight, improving liver health, and boosting overall well-being.
Medical Interventions and Medications
Medical interventions for hepatic cirrhosis aim to address the underlying cause and manage associated symptoms and complications. For viral hepatitis-related cirrhosis, antiviral medications are often prescribed to suppress viral replication and prevent further liver damage. In cases of autoimmune hepatitis, immunosuppressive drugs may be used to dampen the immune response and protect the liver.
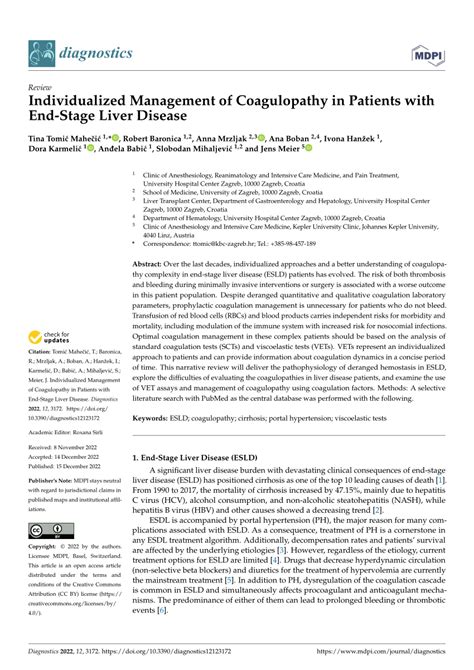
Medications are also available to manage specific symptoms and complications of cirrhosis. Diuretics, for instance, are commonly prescribed to control fluid retention and reduce ascites. Laxatives and certain antibiotics may be used to treat hepatic encephalopathy, a serious complication characterized by mental confusion and altered brain function. Additionally, blood pressure medications may be necessary to manage portal hypertension, a condition often associated with cirrhosis, which can lead to dangerous bleeding in the digestive tract.
Transplantation and Advanced Care
In cases of advanced hepatic cirrhosis, where liver function is severely compromised and the risk of life-threatening complications is high, liver transplantation may be considered. This surgical procedure involves replacing the damaged liver with a healthy liver from a donor. While transplantation offers a life-saving option, it is a complex and major surgery, and individuals must meet specific criteria and undergo rigorous evaluation to be considered eligible.
For those awaiting transplantation or managing cirrhosis post-transplant, ongoing medical care and close monitoring are essential. Regular follow-up appointments with liver specialists, known as hepatologists, are crucial for managing symptoms, preventing complications, and ensuring the long-term success of the transplant. This comprehensive care approach involves a team of healthcare professionals, including surgeons, hepatologists, nurses, and dietitians, all working together to provide the best possible outcome for individuals living with hepatic cirrhosis.
The Future of Hepatic Cirrhosis: Prevention, Research, and Hope
As we look to the future, the landscape of hepatic cirrhosis is evolving, driven by advancements in medical research and a deeper understanding of this complex disease. While there is no cure for cirrhosis, early detection, prompt intervention, and ongoing management can significantly improve outcomes and enhance the quality of life for those affected.
Prevention Strategies
Preventing hepatic cirrhosis is a critical aspect of public health. Education and awareness campaigns play a pivotal role in reducing the incidence of this debilitating disease. By promoting healthy lifestyle choices, such as moderate alcohol consumption and maintaining a balanced diet, individuals can significantly reduce their risk of developing cirrhosis. Additionally, vaccination against hepatitis B can prevent viral hepatitis, a leading cause of cirrhosis, underscoring the importance of proactive prevention strategies.
For those with established liver conditions, early intervention is key. Regular monitoring and prompt treatment of conditions like viral hepatitis and non-alcoholic fatty liver disease (NAFLD) can prevent cirrhosis or slow its progression. This proactive approach to liver health is essential for maintaining overall well-being and preventing the development of life-threatening complications associated with cirrhosis.
Research and Innovations
The field of hepatic cirrhosis research is dynamic, with ongoing studies focused on improving diagnosis, treatment, and management. Researchers are exploring novel therapeutic approaches, including gene therapy and stem cell-based treatments, which offer promising avenues for restoring liver function and slowing disease progression. Additionally, advancements in imaging technology are enhancing the accuracy of cirrhosis diagnosis, enabling earlier intervention and more precise treatment planning.
Clinical trials are also a crucial aspect of cirrhosis research, providing insights into the efficacy and safety of new medications and treatment protocols. These trials offer hope for individuals living with cirrhosis, as they not only contribute to medical advancements but also provide access to cutting-edge treatments that may not yet be widely available.
Hope for the Future
While hepatic cirrhosis remains a significant health challenge, the future outlook is promising. The combination of early detection, improved treatment options, and ongoing research offers a brighter horizon for those affected by this disease. With continued advancements in medical science and a commitment to public health education, we can envision a future where hepatic cirrhosis is managed effectively, and individuals can lead fuller, healthier lives.
Can hepatic cirrhosis be cured?
+While there is no cure for hepatic cirrhosis, early detection and prompt intervention can effectively manage the disease and slow its progression. Lifestyle modifications, medical treatments, and, in severe cases, liver transplantation can significantly improve outcomes and enhance the quality of life for those affected.
What are the early signs of hepatic cirrhosis?
+Early signs of hepatic cirrhosis can include fatigue, loss of appetite, and weight loss. As the disease progresses, more severe symptoms may arise, such as jaundice, fluid retention in the abdomen, and mental confusion. It’s important to seek medical attention if any of these symptoms are present, as early diagnosis is crucial for effective management.
How is hepatic cirrhosis diagnosed?
+Diagnosis of hepatic cirrhosis involves a comprehensive medical evaluation, including a review of medical history, physical examination, and a battery of diagnostic tests. Blood tests, imaging studies, and, in some cases, a liver biopsy may be used to confirm the diagnosis and assess the severity of the disease.



